Verdicts & Settlements
Dan and Kathy Janatik v. Advocate Health Care Network, et al. Jury Verdict: $17,555,957.00 ($16,535,958.00 in compensatory damages for Dan Janatk, and $1,019,999.00 to Kathy Janatik in loss of consortium)
MEDICAL MALPRACTICE In this extraordinarily complex medical malpractice matter, a 30 year old father of two underwent a very specialized cardiac surgery known as the Ross-Konno procedure. In a Ross-Konno procedure, a patient's own pulmonary valve is used to replace his stenotic aortic valve, and a cadaveric pulmonary valve is used to replace the "transplanted" pulmonary valve. During the procedure, Heparin, an anticoagulant, is administered to thin the blood and prevent clotting as the blood contacts the heart lung bypass machine. During the process of weaning the patient from the heart lung bypass machine near the end of the surgery, Protamine, a pro-coagulant, is administered to reverse the effect of the Heparin and restore the body's clotting process. Mr. Janatik's Operative Report suggested that at the time of the re-warming of the heart and weaning from cardiopulmonary bypass machine, a bleeding point was discovered along the suture line at the floor of the right ventricular outflow tract which did not appear to be holding the appropriate stitches. Thrombin, another pro-coagulant, was administered in attempt to stop the bleeding; however, it was determined that it was necessary to return on cardiopulmonary bypass to repair the sutures that came apart. Suctioning of the pro-coagulants (Thrombin and Protamine) should be to a garbage receptacle in the wall using a suction designated for that purpose. Another suction device returns blood to the cardiopulmonary bypass machine. We contended that clots formed in the cardiotomy reservoir component of the heart lung bypass machine due to a surgical error in suctioning the pro-coagulants back into the machine instead of to the garbage receptacle in the wall, and that the tainted blood and clots were injected back into Dan's circulatory system. Dan suffered two distinct points of damage: a large cerebral infarction (death of tissue) to virtually the whole left side of his brain causing right sided hemiplegia; and a spinal infarction causing paraparesis. The damage caused incontinence of bladder and bowel, cognitive impairment, central pain syndrome and a major depressive personality disorder of organic origin. The Janatik family originally contacted the office only two months before the statute of limitation was to run. Because of the short window before the limitation period, I almost did not take the case. It is often the courage displayed by working families that inspires an attorney to take up a fight or to keep fighting. Here, the determination, courage and faith of Dan's wife, Kathy, who was fighting desperately for an opportunity for justice, just as she fought every day for the survival of her family, was the inspiration that compelled us to persevere. After obtaining several court orders for production, we discovered changes to the critical heart lung bypass perfusion record. The perfusion record was on a three sheet NCR (no carbon required) form; the white top sheet had entries that were missing on the yellow carbonless copy which should have been a duplicate copy. The insurance company for the cardiothoracic surgeon offered zero dollars to settle. The jury disagreed and returned a verdict in the amount of $17,555,957.00.Estate of Michelle Hollister v. City of Chicago Jury Verdict: $6,000,000.00 (Verdict later reduced for comparative negligence, tort immunity, and joint & several liability) POLICE CHASE - City of Chicago police officers began a chase after a domestic fight between driver Spencer and his girlfriend. The officers in the unmarked vehicle that originated the chase claimed that the Spencer car jumped the curb and had a minor collision with the unmarked police car; although, this story was disputed by the girlfriend. After several miles of chasing the Spencer vehicle through South Side residential neighborhoods, a marked police vehicle struck Michelle Hollister's vehicle in the intersection, killing the 25 year old graduate student. Questions of fact were raised regarding the color of the light at the intersection and whether the marked squad car had its lights and siren on at the time. In this multi-week trial, Mr. Ford looked to the able assistance of his co-counsel, Mr. Byron L. Mason of Hyde Park, marking the second trial the two trial attorneys tried together. The trial court subsequently reduced the $6,000,000.00 award to $540,000.00 base upon comparative negligence, tort immunity, and joint and several liability. The case later settled pending appeal.
Howard and Dorothy Fountain v. Morris Mauer, M,D., et al. Jury Verdict: $5,267,581.00 ($4,462,581.00 compensatory to Howard, $805,000.00 to Dorothy for loss of consortium) (The verdict was reduced by 35% for comparative negligence)
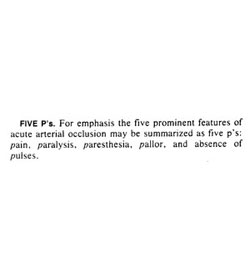
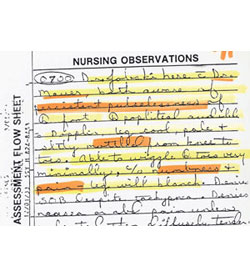
MEDICAL MALPRACTICE Howard Fountain claimed that he went to the defendant internist complaining of right lower quadrant pain. The defendant doctor claimed that the patient was seen only for a refill of prescriptions for a heart condition, diabetes, chronic obstructive pulmonary disease, peripheral artery disease and gallstones. Two months later, Howard Fountain returned with a similar complaint and was diagnosed with gallstones. Howard's symptoms persisted, and after another month passed, he was admitted to the hospital with unbearable abdominal pain, fever and vomiting, which again was initially diagnosed as being gallstones by the internist. Five hours into his hospital admission, it was determined that Howard had a perforated appendiceal abscess which had caused septic shock and hypotension. Twelve hours after admission, an alert intensive care unit nurse observed Howard's leg, identified and noted the "5 Ps of Acute Arterial Insufficiency": pain, pallor, paresthesia, paresis and pulselessness. Notwithstanding, no vascular surgery consultation was given to Howard for several weeks, by which time, compartment syndrome and gangrene had set in. Howard required an above-knee amputation. The defense hired as their expert, Dr. Seymour Schwartz, who was the editor of the two major textbooks on Surgery. We found excerpts from Dr. Schwartz' textbooks supported the plaintiff's theory of the case, to wit, that the condition should have been diagnosed due to the clear nursing documentation of the "5 Ps of Acute Arterial Insufficiency" - pain, pallor, paresthesia, paresis and pulselessness. The insurance company for the physician offered zero dollars to settle the case, asserting that it was the plaintiff's fault for failing to seek medical attention in the weeks preceding his admission. The jury respectfully disagreed and returned a verdict on behalf of Mr. and Mrs. Fountain in the gross amount of $5,267,581.00.Theodore Schaumburg v. Provena Hospital and Diane Solis, M.D. Jury Verdict: $4,752,000.00 (Kane County)
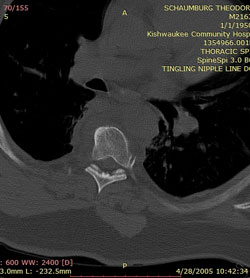
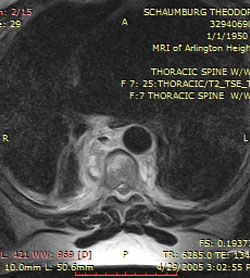
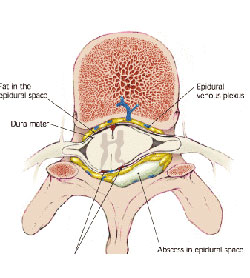
MEDICAL MALPRACTICE Theodore Schaumburg presented to the emergency room at Provena Hospital on April 9, 2005 with a primary complaint of back pain that originated behind his right shoulder and radiated around to his chest. The original treatment plan was to admit Ted to the hospital and rule out any possible cardiac arrest, and then, if the tests came back as negative, to treat Ted for possible musculoskeletal sources of pain. During the course of Ted's admission, his blood work showed a "shift to the left" on the Complete Blood Count with Differential, as well as an extremely elevated Erythrocyte Sedimentation Rate, both indications of infection in progress. A low grade fever also was present. Ted’s cardiac lab results came back negative, confirming that the cause of the back pain was not the heart. However, other lab results also showed an elevation of myoglobin enzyme levels, which is a reflection of a muscle enzyme which is present when muscle fibers dies. The physicians attributed the excessive myoglobin level – a condition called rhabdomyolysis - to Ted’s use of the anti-cholesterol statin, Lipitor. Ted began to experience difficulty eliminating feces, and he continued to express severe back pain, despite the fact that he was being administered morphine to manage the pain. A CT scan of the thorax and abdomen was ordered by one of the admitting physicians. Unfortunately, because of a hospital clerical error, the primary reason for the CT scan was incorrectly communicated as “chest pain” instead of “back pain.” Therefore, the CT scan protocol was changed to focus on the lungs and aorta, and the necessary digital information regarding the back and spine was not captured by the study. No spinal study was performed despite the fact that the primary presenting complaint was back pain. The radiology study that was performed did show abnormalities in the area of his posterior thoracic region, specifically, a fluid build-up in the pleural lining behind the lung and compressive atelectasis, a collapse of part of the parenchyma of the lung. These changes were assumed to be pneumonia, instead of a fluid reaction to the infectious process occurring in the adjacent paraspinal area. Throughout Ted's admission, Ted's care was managed by his primary care physician, Dr. Diana Solis. Dr. Solis was unaware of Ted's primary complaint of back pain throughout his admission, despite numerous notations by nurses and consultant physicians. Dr. Solis dismissed Ted's inability to defecate, and discharged him home on April 15, 2005 with diagnoses of pneumonia and rhabdomyolysis. Following his discharge, Ted continued to have an inability to defecate, and his back pain symptoms were exacerbated with "shock" sensations shooting down his spine and through his legs which caused him to fall to the ground on multiple occasions. Ted placed calls to Dr. Solis on April 18 and 20 concerned with the constipation – Ted’s symptoms were excused and Ted was told to try over-the-counter digestive aids. On April 22, 2005 Ted presented for an appointment in Dr. Solis' office with continued complaints of constipation, back pain, and "shock" sensations into his legs. Ted testified that without performing a physical exam of Ted's back, Dr. Solis prescribed a muscle relaxant and pain medication to Ted and sent him home. Dr. Solis denied being told about the back pain shooting down the legs, denied ascribing the pain to muscle spasms, and denied prescribing pain medication and muscle relaxants to Ted, noting that there was no mention of either in her medical records. When plaintiff’s counsel produced the prescription bottles for the pain killer, Ultracet, and muscle relaxants, Cyclobenzaprine, Dr. Solis suggested that perhaps the medications were simply re-fills for past back problems relating to golfing. On April 27, after being unable to defecate for nearly two weeks, Ted again called Dr. Solis, expressing concern over the ineffectiveness of the over-the-counter constipation medications she had told Ted to use. Dr. Solis recommended another over-the-counter medication, and told Ted to call back in 48 hours. The next day, April 28, 2005, Ted called Dr. Solis desperate, as he had been unable to produce a bowel movement for nearly 2 weeks. Dr. Solis, referred Ted to a gastroenterologist, and that evening, less than an hour after having his consultation, his legs collapsed underneath him. Ted arrived at the emergency room by ambulance. By the time he reached the emergency room, Ted was paralyzed from his nipple-line to his toes. An MRI established that the cause of Ted’s paralysis was a paraspinal, epidural abscess at the thoracic level of his spine, the level of his shoulder, exactly where he was complaining of pain one month earlier. The fibrous nature of Ted's spinal abscess indicated that the process had been developing over an extended period of time and was the most likely cause of the symptoms Ted experienced during his admission to Provena Hospital from April 9, 2005-April 15, 2005 two weeks earlier. Had appropriate communication, evaluation, and diagnosis been provided during the period beginning on April 9, 2005 through the onset of Ted's neurological deficit, Ted's abscess could have been treated with antibiotic therapy, and his paralysis would have been averted. The insurance company for Dr. Solis offered zero dollars to settle. The jury in one of the most conservative counties in Illinois decided to differ with the insurance company’s assessment and returned a verdict in favor of Ted in the amount of $4,752,000.00.Karen Holliday v. Certain Confidential Medical Center Settlement on Eve of Trial: $4,500,000.00
MEDICAL MALPRACTICE When Karen Holliday, a 56 year old African-American woman, caught her foot in the carpet and lurched forward a little, she felt her arm fall out of place. She was diagnosed as having a subluxation with shoulder effusion, and x-rays revealed a lesion in the metaphysical region of the left humerus demonstrating a permeative pattern with wide zone of transition and questionable cortical breakthrough. The lesion appeared aggressive. The description was consistent with a metastatic growth. Subsequent radiologic examinations concurred with this interpretation. The plan at the time of the surgery, assuming the biopsy showed a primary cancer, was to give neoadjuvant chemotherapy and/or radiation to kill some of the cancer cells before surgery followed by wide excision, shoulder amputation, or cancer type amputation. However, the pre-surgical biopsies of the lesion were conflicting: one suggestive of Giant Cell Sarcoma cancer and one suggestive of Giant Cell Tumor of Bone (a benign process). A resection of the left proximal humerus with medulla oncology prosthetic reconstruction, an incorrect surgery for a cancerous process, was performed. The post-surgical pathology samples demonstrated a cancerous process; however, the pathology report was not timely delivered to the treating physicians. Four months later, an MRI showed the recurrence of the mass. A forequarter amputation was performed to attempt to stop the spread of the cancer; unfortunately, it was too late.Estate v. Roney Oatman, Inc. Settlement on Eve of Trial: $4,375,000.00 (Kane County)
TRUCK COLLISION The plaintiff's decedent was operating his car on a country road in rural McHenry County when he collided with an ice cream delivery truck. An eye witness identified by the defendant claimed that the car was speeding at a high rate of speed, and that the defendant truck driver had stopped and carefully pulled into the intersection. Our accident reconstruction expert interpreted the road markings at the scene of the incident and determined that the defendant's truck was traveling at a high rate of speed, a theory that would be inconsistent with his claim of stopping his truck at the stop sign governing traffic at the intersection. Subsequently, we discovered the truck maintenance records for the vehicle and deposed the head of maintenance for the company who testified that because the new owners had been cutting back on overhead, the maintenance department could not keep up with the maintenance on the vehicles.Jozef and Anna Sobczak v. Joseph Flaska Jozef and Anna Sobczak v. Providence Washington Insurance Co. Jury Verdict: $3,600,000.00 ($3,125,000.00 compensatory to Jozef, $475,000.00 to Anna for loss of consortium)
CONSTRUCTION WORK SITE INCIDENT Jozef Sobczak was working on a garage construction project at Flaska's home. As he was unloading heavy equipment from a flatbed trailer using a Case 350 crawler, the crawler slid off the side of the trailer. When Jozef tried to leap free, his leg was pinned under the tracks of the crawler, and he later required an above-knee amputation. The crawler was 20 years old and had been re-assembled shortly before the incident by Jozef who had learned about tractors as a farmer in Poland. The tractor did not have any rollover protection device. (The machine was manufactured only weeks before such devices became a mandatory requirement for the manufacturers.) We alleged that Flaska as homeowner and general contractor on the construction site had a duty to provide a rollover protection system on the crawler. The homeowner defendant had written his insurance company, Providence Washington on several occasions asking the case be settled within the $300,000.00 homeowner’s policy. The insurance company did not respond to the correspondence, choosing instead to offer $25,000.00 to settle and withdrawing the offer by letter later the same night. After the jury returned a $3,600,000.00 verdict, we pursued a "bad faith" insurance contract lawsuit against Providence Washington Insurance Company. Ten years to the day the crawler fell on Jozef's leg after multiple appeals and the prosecution of the bad faith claim - we were able to recover almost the full amount of the jury's verdict. Mr. Ford was assisted at trial by Hyde Park attorney Byron L. Mason, marking the first of several trials the two trial attorneys have tried together.Keith P. vs. Confidential Manufacturer of Industrial Equipment Jury Verdict: $3,079,000.00
PRODUCT LIABILITY Keith P. grew up on the tough streets of Maywood, Illinois. After initially dropping out of school, Keith persevered to obtain his GED degree, attend college, and then obtain work as a highly skilled chemical operator at ICI Uniqema, a manufacturing plant on the Southwest Side of Chicago, in the old Stockyards district. ICI Uniqema produced of glycerin and distilled fatty acid products in a process using a catalyst – nickel – which separates or distills the animal fat into steric acid, fatty acid, oleic acid and glycerin which are loaded into tankers and sold to other manufacturing concerns. Working on the night shift of February 8, 2005, Keith was operating a forklift to load large 1400-1500 pound bags of spent nickel catalyst (the waste product from the chemical reaction) into a disposal dumpster. As he lowered a bag into the hopper, it came out of position on top of another bag. In order to close the dumpster, Keith had to adjust the bag, so he attempted to do so with a chain attached to the bag. In the process of adjusting the bag, the forklift tipped forward on to its front wheels forcing Keith’s body forward, pulling on the seat belt that he was wearing. The seat is mounted on the forklift’s engine hood. The hood is intended to be secured to the body of the forklift by a single hood latch configuration. The engineering intent is that with the hood properly latched, a belted operator would remain safe within the safety zone of the overhead protection. Unfortunately, on the evening of the incident, the hood latch was not properly aligned and therefore did not latch; thus, when the vehicle tipped it caused the unlatched hood and seat -with Keith on it - to rotate up and forward. Keith lost his ability to brace his legs, causing his right leg to be come out to the side of the forklift where it was crushed by the forklift as it fell over to its side. Keith sustained severe crushing injuries to his right foot and ankle, ultimately requiring a below-knee leg amputation, as well as facial fractures to his maxilla (upper jaw) and four teeth, which were sheared off when his face struck the pavement in the “flyswatter” effect as the forklift fell on its side. During the investigation and discovery in the case, we discovered that the manufacturer had changed the design of the latch assembly to remove the “tolerance” or “play” in the latch device. The manufacturing “tolerance” is necessary to account for any deviations in manufacture. The design change documents identified the reason for the design change as a “cost reduction”. Thus instead of having ¼ inch room for error in the design, the piece had no room for manufacturing deviation. The evidence also demonstrated that during the assembly of the forklift, the inspector on the line found the “hood & valve cover way off.” Although that inspector could not recall what he specifically did in this case to correct the hood being “way off,” somewhere five washers had been placed in the hinge of the hood of forklift. The five washers displaced the alignment of the hinge 0.2849 inches, forcing the latch fully out of alignment. At trial, we asserted the forklift truck was defectively designed and manufactured, in that its hood assembly failed to secure the hood and seat in the closed position. The defense denied any defects and contended Keith attempted to jump out of the seat and run under the falling mast of the forklift during the tip-over, only to have the forklift mast strike and crush the back of his leg. To defend the case, the manufacturer hired a formidable team of attorneys, including two of the largest defense firms in Chicago and top trial attorneys from Philadelphia. The manufacturer also hired five highly paid experts to rebut plaintiff’s claims, including one expert who they paid in excess of $150,000.00 before the expert even entered the courtroom for trial. Because of the massive amount of documentation and exhibits, solo attorney Mr. Ford relied on the assistance of his paralegal, Michelle Konieczki, and the help from his old friend, Byron L. Mason, an attorney from Hyde Park who tried the case with Mr. Ford. This was the third verdict the team of Ford and Mason have obtained together. The confidential manufacturer of industrial equipment offered Keith zero dollars to settle. The jury disagreed with the manufacturer’s assessment of the case and returned a verdict in the sum of $3,079,000.00. The verdict was settled in the post-trial period before appeal, pursuant to a confidential settlement agreement.Robert Carter v. Chicago Antique Brick Company, et al. Jury Verdict: $2,985,649.54
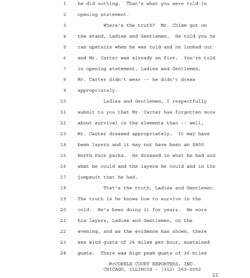
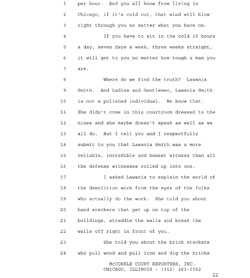
CONSTRUCTION SAFETY - Robert Carter was 17 years old when he volunteered, with his mother's consent, for the United States Marines. After returning from his service in Viet Nam, Robert worked as a day laborer in the de-construction or construction demolition industry. On the night of January 22, 2002, Robert was working as a night watchman at a demolition site located at Bell and 35th Street in Chicago, Illinois where he was watching valuable, reclaimed antique bricks. After the Great Chicago Fire on October 10, 1871, Chicago's brick industry blossomed as Chicago re-built its buildings and homes with brick instead of wood. Chicago bricks from this epoch are considered to be higher quality and better looking than modern bricks. Many of the turn of the century buildings' and factories' most valuable assets are the bricks themselves. The defendant corporations were in the profitable business of reclaiming and selling used bricks from demolition sites. Demolition is a messy process. The bricks are "reclaimed" thanks to the hard work of day laborers hired to climb, straddle and tear down the walls using saws and crowbars, then later, sift through the wreckage and clean, sort and stack the bricks. These workers are known in the industry as "brick-stackers." Brick stackers are paid a flat rate of approximately $l0.00 cash per 1000 bricks stacked. Brick stacking is backbreaking work - the average stacker can complete maybe 2000-3000 bricks per day, clearing 20-30 dollars a day, perhaps twice as much if they work 10-12 hour shifts. The brick reclamation company, who essentially obtains and finances the jobs, turns around and sells the bricks to retail brick dealers for $300.00 per 1000 bricks. The retail brick dealers then sell the antique bricks to home builders for $600.00 per 1000 bricks. The worksite in question generated over $30,000.00 in brick sales. Robert Carter's job, in the instant case, was performed in December-January in the blinding cold and winds of Chicago winter. The only heating equipment provided to workers was a 55 gallon drum, commonly referred to as a fire barrel, and the timbers that lay around the site from the demolition. On the evening of the incident, there were sustained winds of 26 m.p.h. and wind gusts of 36 m.p.h. Robert was paid $50.00 cash to work from 4:00 in the afternoon, through the dead of night, until 7:00 or 8:00 the following morning in Chicago's January weather conditions. Robert worked 15-16 hours per day, 7 days per week under these conditions. Around midnight on the evening of January 22, 2002, Robert's clothes were ignited as he attempted to stay warm by the fire barrel provided to him, and he was severely burned. We argued that the brick reclamation company should have provided a simple shelter and a $60.00 propane heater in recognition of Robert's basic humanity. The brick reclamation company argued that Robert was an unknown, homeless person who snuck onto the property to start a fire in the fire barrel to keep warm and offered zero dollars to settle. The jury disagreed and returned a $2,935,650 verdict.Estate of Urszula Lewicki v. Our Lady of the Resurrection Hospital, et al. Settlement on Eve of Trial: $2,750,000.00
MEDICAL MALPRACTICE Urzsula Lewicki, a 33 year old immigrant from Poland, and her daughter, Magdelena, were watching a movie "Stepmom" (a movie about a mother who had cancer, was dying and leaving children behind) when Urzsula became upset and short of breath. She stepped outside where she began to experience substernal chest pain. Mrs. Lewicki presented to the emergency room of Our Lady of the Resurrection Hospital, where an ECG was performed. The computer read the ECG as abnormal, evincing: (1) marked sinus bradycardia of 45 beats per minute; (2) low voltage QRS; and (3) a septal infarct, age undetermined. The emergency room physician, after obtaining a history and performing a physical exam, did not feel that ordering a cardiac profile panel was necessary, and Mrs. Lewicki was discharged with a diagnosis of hyperventilation induced chest pain with a prescription for Xanax to quell anxiety. We believed that the hospital and physician failed to diagnose and treat an acute coronary syndrome caused by a partial dissection of the left coronary artery. Three days after her trip to the emergency room, on May 12, 1999, Mrs. Lewicki sustained a complete dissection of the coronary artery causing full cardiac arrest and death. The hospital retained numerous experts who claimed there was no evidence of cardiac infarction or hypoxia at the time of the earlier examination. We were able to prove, through microscopic cardiac pathology, that there were inflammatory cells in the myocardium of the heart that could only be present as the result of a cardiac event 2-3 days preceding the death.Noah, a minor v. Michael Detweiler, D.C., et al. Settlement on Eve of Trial: $2,000,000.00
CHIROPRACTIC MALPRACTICE /NUTRACEUTICAL PRODUCT LIABILITY Noah sustained a condition called hypervitaminosis from the overdose of Vitamin A, resulting in liver damage, bone growth abnormalities and certain developmental delay. Michael Detweiler, D.C., in the course of his professional services as a chiropractor at the Detweiler Family Chiropractic Clinic, formerly located in Eureka, Illinois, prescribed doses of Vitamin A supplements in amounts as much as 6,000 times the daily recommended adult dose to Noah, then an infant of 9 months old. The vitamin supplement in question was a form of Vitamin A derived from animals known as Pre-Formed Retinol Palmitate (meaning that it had already been processed in the digestive system of some animal) rather than a plant source or Pro-Vitamin Carotene source of Vitamin A. Excess Pro-Vitamin Carotene Vitamin A will be excreted by the natural processes in the human body. The Retinol Palmitate form of Vitamin A can accumulate in the liver and lead to toxicity, as it did in this child.Marcin Wierciszewski v. MOBBA S.C.C.L. , et al. Settlement on Eve of Trial: $2,000,000.00
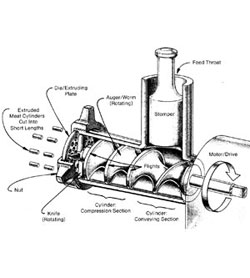
PRODUCT LIABILITY - Andy's Deli had two meat grinders on their premises. Neither meat grinder had any hand safety device or warning signs or symbols. In fact, there was an optional hand protective guard for the machines; however, the guard could be readily removed by unscrewing two wing nuts. The owner testified that he had seen advertisements showing the machine without the guard, which indicated the machine could be used without the guard. The distributor's owner, engineering supervisor, sales supervisor and marketing supervisor all acknowledged that the machine was advertised without the guard but did not know why the machine is advertised without a hand guard. There was a dispute as to how the machine made its way into the hands of the deli without warning signs and symbols. However, there was evidence showing that the machines may have been used as display models at a manufacturers' sales convention at McCormick Place in Chicago, where there has long been an unfortunate custom of removing warning signs and symbols, so as not to scare off potential retailers from placing wholesale orders. Table top meat grinders operate such that large chunks of meat are dropped into the feed throat toward a rotating auger within the body of the grinder. The food is crushed between rotating flights which convey the meat through a cylinder section where it is pressed against a die, resulting in spaghetti-like cylinders. Ground meat is normally passed through a meat grinder two times. On the second pass, the meats tensile strength is reduced, so it must fall or be pushed through the feed throat, with a stomper, if one is made available to the worker. Where no stomper is made available, as in the instant case, the worker will use his hand. Marcin, who had only recently immigrated from Poland, had only been working at the establishment for a few weeks. Marcin was instructed to always grind the meat twice and to feed the machine by hand. Marcin mistakenly believed that the machine was somehow safeguarded for this use. While pushing the meat into the feed throat, Marcins hand was sucked in and ripped off.James Stallworth v. Michael Reese Hospital, et al. Settlement on Eve of Trial: $1,850,000.00 MEDICAL MALPRACTICE James Stallworth was a 74 year old man who underwent a neck surgery to cure numbness in his hands. When his neck became so painful that he could barely move his neck, an MRI was performed. It was read as essentially normal. A week later, Mr. Stallworth went to the hospital for physical therapy treatment. At the end of his session, as he sat up and put on his coat to leave, Mr. Stallworth experienced an excruciating pain in his neck which caused him to lose the use of all four of his extremities. The event rendered him an "incomplete quadriplegic"; he lost use of his legs and had limited use of his arms. Mr. Stallworth's physicians told him that he had suffered a stroke. Two and one-half months before the statute of limitation ran, friends recommended that he look into the care he had received. Because there were no lawyers in his South Side neighborhood, Mr. Stallworth and his wife of 50 plus years contacted the Chicago Bar Association who, in turn, put him in touch with our office. Our neuroradiologist stated that he interpreted the MRI as showing a subluxation at C1-C2, a "hangmans fracture", which he believed was due to post-surgical infection. Three years after fighting in the case, during a court ordered inspection of the original radiology file at the hospital, we found a paper reference to x-rays taken around the time of the MRI that had interpreted the neck as normal. This cervical spine report and the x-rays had never been produced. Upon receiving the films, we found that the cervical spine x-ray films demonstrated a clear picture of a subluxation, known as a hangmans fracture, resulting from a post-surgical infection eating away at the spine at the C1-C2 region.
Kheath Kem v. Commonwealth Edison Settlement after defeating Summary Judgment: $1,800,000.00
ELECTRIC POWER LINES Kheath Kem was imprisoned with her brother, both orphaned children, in a concentration camp in Cambodia during the era of the "Killing Fields" of Cambodia. Kheath was protected and cared for by a former Colonel in the Cambodian Army. The night before the execution of prisoners in the concentration camp, a soldier still loyal to the Colonel who was acting as a guard for the camp warned the Colonel and arranged for the guards to look the other way as the Colonel, Kheath and her brother slipped through the barbed wire of the concentration camp in the middle of the night. Eventually, Kheath and her brother settled with other Cambodian immigrants in the Southeast Asian neighborhood on the North Side of Chicago. She attended church at the Wheaton Chinese Alliance Church - which at that time was located in a rural portion of DuPage County. Kheath and her friends decided to pick some apples from a stand of apple trees found on the church lot. Unbeknownst to her, a 7200 volt power line ran through the middle of the tree, and she was electrocuted and became paraplegic. The case came to us after most of the apple tree had been cut down, apparently destroying the evidence. The power company and tree cutting employees claimed that the power line was obvious to anyone in the area because the tree was V cut around the line. However, we hired an expert arborist from the famed Mortons Arboretum, who, in conjunction with a commercial artist, reconstructed the tree and the re-growth that would occur after a V cut relative to the electric wire by basing the reconstruction on the remaining tree trunk and logs which were present at the time a photographer was able to take photos of the site. The case was settled shortly after Commonwealth Edison was denied summary judgment on the then developing Illinois legal theory of open and obvious dangerEstate of Vernon Banks v. West Suburban Medical Center Settlement: $1,600,000.00 on the eve of trial
Vernon "Chico" Banks was one of Chicago's great Blues Guitarists. The Chicago Blues Guide says: "As a solo artist, Chico Banks played the blues in his own, very contemporary, way with a dose of funk, sould, rock and R&B. The son of West Side Blues/Gospel musician, Jesse Banks... Chico Banks was a guitar prodigy who could play in a variety of styles, which made him a sought after sideman for an eclectiv array of Chicago musicians for both their live and studio bands. Starting at age 14 in a Top 40 band, Chico's talent was noticed by the late singer Johnny Christian, who first hired the teenager. The guitarist went on to work in touring bands with Otis Clay, Buddy Guy, Junior Wells, James Cotton, and Artie "Blues Boy" White..." From November 14-21, 2008, Chico was admitted at West Suburban Medical Center with a history of fever, chills, elevated white blood cell count and anemia. Importantly, Chico had had a recent porcine heart valve replacement. Chico's week long admission revealed non-reassuring blood tests and an unexplained fever. Infective endocarditis is an infection of the endocardial surface of the heart and may include the heart valves. It can lead to severe valvular insufficiency, intractable congestive heart failure, myocardial abscesses and death. The infection will cause embolic vegetation around the heart valves. Should these vegetations break free and travel in the circulatory system, they will travel to internal organs where they lodge in the vessel, cut off blood flow, and result in infarction or death of tissue. Radiology studies on admission revealed infarctions in the spleen. Of primary concern in infective endocarditis is that if vegetation/embolic material break free and travel to cerebral blood vessels, infarction or "stroke" of brain tissue will result. The risk of stroke in infective endocardits falls dramatically after the initiation of effective antimicrobial therapy for one week. We argued that had the gold standard diagnostic tool of transesophageal echocardiogram been ordered, along with serial blood cultures and infectious disease consult, the infective endocarditis would have been diagnosed, the appropriate antibiotics given and Chico would have survived. Instead, Chico was discharged on November 21, 2008 with a diagnosis of Acute Gastritis. On November 29, 2008, Chico sustained an embolic stroke, passing away days later.Georgia v. Kloos Settlement: $1,600,000.00 AUTOMOBILE COLLISION. Automobile collision in Tinley Park, Illinois resulting in the death of a mother.
Estate of Anita James v. Neubauer Settlement for Full Policy Amount: $1,500,000.00 AUTOMOBILE COLLISION Intersection incident with disputes regarding color of the light and right of way, resulting in the death of a 22 year old single woman
Joanne Matthews v. Northwestern Memorial Hospital and NW Faculty Foundation Settlement: $1,500,000.00 on the eve of trial
MEDICAL MALPRACTICE: Joanne Matthews worked as a Licensed Practical Nurse for over 30 years. In April 2011, radiology studies found a mass in her abdomen and a mass on her left kidney. A follow-up biopsy showed the abdominal mass was consistent with a non-cancerous leiomyoma (commonly referred to as a “fibroid”). Approximately 99% of the time, a leiomyoma is benign. The Northwestern Memorial Faculty Foundation surgeon counseled Joanne that, despite the biopsy result suggesting that the abdominal mass was benign, the mass could still be a malignant sarcoma, and recommended an exploratory laparotomy. No follow-up was performed on the kidney lesion. An exploratory laparotomy surgery was performed, and the pathology results again confirmed that the abdominal mass was not cancerous. There were no complications reported by the surgeons in the Operative Report, and no reference was made regarding any damage to the small bowel. Subsequent to this first surgery, Joanne became extremely sick, developing severe abdominal pain and a small bowel obstruction, a serious condition which precludes fecal matter from passing. A second exploratory laparotomy was performed two weeks later, and the Operative Note indicated that a small length of small bowel of 12.5 cm (5 inches) was removed to treat the small bowel obstruction. After the second surgery, Joanne became sicker yet, with severe abdominal pain and small bowel obstruction persisting, and with a new development of abdominal abscesses, sepsis, and a dehiscence of her abdominal closure (the scar opened up), resulting additional surgeries to remove gangrenous small bowel and to close the wound. During the legal proceedings, we discovered photographs in the Pathology Department of the surgical specimens from the second surgery which contained not just one small length of bowel, but rather “two segments of small intestine measuring 12.5 cm in length and 63 cm (25 inches) in length” - at odds with the Operative Report of the second operation that only referred to the smaller length of bowel being removed. In the unreported 25 inch length of small bowel, there were multiple sutured, transmural defects with fibrinous inflammatory exudate. In other words, there was a 2 foot length of small bowel which had been cut through all its layers which had suture repairs with a fibrinous process around the sutured areas that would take approximately two weeks to develop. Our pathology and surgical experts testified that common sense dictates that the small intestines were inadvertently cut during the first surgery and not reported in the Operative Report of the first surgery. During the repairs of the second surgery, the 25 inch length of small bowel containing the sutures from the first surgery similarly went unreported in the Operative Report of the second surgery. Topping things off, the kidney lesion which was not followed up on originally turned out to actually be cancer. Treatment of this cancer by an urologist was delayed due to the months it took Joanne to recover from the injuries sustained on the exploratory surgeries on what was a benign mass in the abdomen. Joanne developed a “surgical abdomen” with severe abdominal adhesions (internal scarring binding up her intestinal tract) that caused a severe neuropathic pain syndrome in the abdomen.Estate of Elsa Gonzalez v. St. Anthony Hospital Settlement: $1,300,000.00 MEDICAL MALPRACTICE The physician failed to properly identify and treat pre-eclampsia and eclampsia, which resulted in the mother's death during labor and delivery. The case came to us after several other attorneys had turned the parents down, asserting there was no case.
Estate of Juan Antonio Lopez v. St. Anthony Hospital, et al. Settlement on Eve of Trial: $1,200,000.00 MEDICAL MALPRACTICE Juan Antonio, a 15 year old, was playing basketball with his brothers in the back yard when he experienced lightheadedness, blurring vision and a fall, possibly fainting. His parents, immigrants from Mexico, took Omar to a pediatric cardiologist who inaccurately read his echocardiogram and stress testing as normal and discharged him without providing any explanation of his syncopal event. His echocardiogram actually demonstrated an enlarged right ventricle, and his stress test actually demonstrated an "R on T" phenomenon which occurs when a patient has a premature ventricular contraction on the T wave, which increases the odds of ventricular fibrillation. Shortly thereafter, Omar was playing basketball at a local boys club when he had a fatal heart attack, collapsed and died. The heart was sent for study to a renowned physician at the Heart Institute for diagnosis, who incorrectly diagnosed the condition as "Uhls Anomaly", an incurable disease. Our investigation later revealed that that physician from the Heart Institute and the defendant physician were old colleagues, who had previously written medical articles together. An alert member of the Medical Examiner's office caught the super specialist's "error" and correctly diagnosed the condition as a treatable, yet serious, congenital heart condition known as Arrhythmogenic Right Ventricular Dysplasia. Our expert cardiac pathologist confirmed the Medical Examiners testimony by his review of the microscopic slides.
Cartyiel Timmons-Williams v. A Certain Confidential Hospital Settlement on Eve of Trial: $1,200,000.00 plus waiver of liens MEDICAL MALPRACTICE Cartyiel Timmons Williams was born significantly premature, at twenty-six weeks, and spent his initial 11 months in a hospital due to severe bronchopulmonary dysplasia and ventilator dependency. Pre-incident testing showed that Cartyiel had significant developmental delay. At 11 months, Cartyiel was transferred to a major teaching hospital due to bronchospasms and cyanotic spells. During the hospitalization, Cartyiel suffered a cardiac arrest. In discovery we learned that Cartyiel's tracheotomy had dislodged, disconnecting him from the ventilator, and that the event caused a lack of oxygen, which in turn caused the cardiac arrest. The hospital took the position that it was impossible to distinguish any injury that occurred from the cardiac arrest, asserting that Cartyiel suffered from pre-existing brain damage due to prematurity and ongoing anoxic insult from his lung condition.
Estate of Koffarnus v. Poole Truck Lines Settlement on Eve of Trial: $1,350,000.00 TRUCK COLLISION Mr. Koffarnus, a 43 year old divorcee with two adult children, and his partner were operating a truck and entering I-55 near Cape Girardeau, Missouri, when his truck rear ended a Poole Truck Lines truck. Poole Truck Lines' driver claimed that Mr. Koffarnus was operating his vehicle at a high rate of speed entering the highway. Our accident reconstruction expert interpreted the road markings and determined that the Poole Truck Lines truck initially moved to the left and then prematurely swerved back into the right hand lane as Mr. Koffarnus was entering the highway, cutting off his merge path. The collision resulted in the death of both Mr. Koffarnus and his partner.
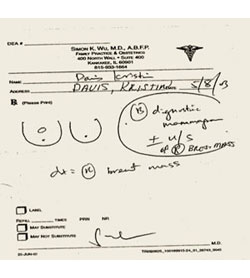
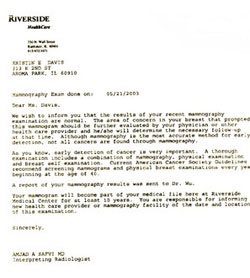
Kristen Davis v. Riverside Medical Center, et al. Settlement on Eve of Trial: $1,150,000.00 (Kankakee County)
MEDICAL MALPRACTICE Kristin's symptoms began shortly before May 8, 2003, when she was 37 years of age. Kristin presented to her primary care physician, Dr. Wu, with complaints of a protruding lump on the top of her breast, a palpable right breast mass. Dr. Wu believed that the lump was a benign cyst but sent Kristin for mammography and ultrasound at Riverside Medical Center in Kankakee, Illinois. The ACR Guideline for the Performance of Diagnostic Mammography, ACR Practice Guideline, effective 01/01/03, states in relevant part: "Diagnostic mammography is a radiographic examination performed to provide additional information about patients who have signs and/or symptoms of breast disease, radiographic findings of concern, or in situations where direct supervision* of the imaging is deemed appropriate by the interpreting physician." *Direct Supervision is defined as the physician being present and immediately available to furnish assistance and direction throughout the performance of the procedure. The radiologist, Dr. Safvi, normally arrived at the hospital 08:00-09:00 a.m. The mammogram report shows on its face that Kristin's mammogram was performed at 07:04 a.m., well before Dr. Safvi would normally arrive at the hospital to supervise. The mammography films were read by the radiologist as questionable and called for additional studies. The ultrasound was interpreted as negative. Even though the presenting history was of a palpable mass at the 11:00 o'clock position, the case was signed out as a Category 1 negative with no recommendation for follow-up. The cancer was diagnosed eleven months later on April 1, 2004, after the cancer had grown from a Stage I mass to a Stage III mass. We argued, inter alia, that those additional studies should have included a spot compression film that would have been diagnostic of the mass.Freddie Palomares v. Nasir Yaqub, M.D. et al Settlement on Eve of Trial: $1,150,000.00 MEDICAL MALPRACTICE The physician failed to properly identify and treat neonatal seizures, which resulted in neurological injury. The case was made very difficult because it came to our office nearly 8 years after the birth, and many of the medical records could not be found.
Charles Redd v. Bananas.Com d/b/a Cermak Produce No. 2 et al. Settlement on Eve of Trial for Full Policy Amount: $1,000,000.00 WORK SAFETY - Charles Redd was a "lumper", a freelance dock worker hired to load produce on the defendants’ produce truck at the South Water Market, a wholesale fruit and vegetable market first built back in August of 1925, which, at the time of the incident, was located just South of Roosevelt Road and Morgan Street (just behind the University of Illinois at Chicago swimming pool complex). Because of union regulations, dock workers laboring for the fruit and vegetable companies were allowed to bring the crates of produce to the dock but could not place them in the trucks. The union for the truck drivers would not allow the drivers to load anything from the docks. Accordingly, the lumpers fill the void and, for a negotiated cash price, move the produce from the docks into the trucks trailers. The work would occur in the pre-dawn hours before the city’s restaurants opened for breakfast. Mr. Redd was moving pallets of produce inside the Cermak Produce No. 2 truck when an unguarded and unsecured 45,000 BTU propane heater, used to keep produce from freezing, tipped over and ignited Mr. Redd’s clothing, which resulted in severe burns to 21% of his body. Liability hinged upon whether the propane heater's safety guard had been removed, making the heating apparatus hazardous and in violation of applicable Federal Motor Carrier Safety Regulations. Defendants maintained that Plaintiff was an unwelcome trespasser on the truck. Since the incident, the South Water Market has been converted to townhouses and condos to complement the new University Village townhouses to the east.
Rubin Connor v. Certain Confidential Physicians, et al. Settlement on Eve of Trial: $1,000,000.00 MEDICAL MALPRACTICE Rubin Connor was a 56-year-old African American man with a medical history including Type 2 Diabetes, cerebral stroke with residual right-sided weakness and end stage renal disease secondary to diabetic neuropathy. Mr. Connor’s condition required chronic hemodialysis. Because of an obstruction to the blood flow in his leg, a bypass procedure was performed. During the subsequent five week rehabilitation course, the leg became infected at the surgical graft site, and despite documented positive cultures, CT scans showing an unusual accumulation of fluids at the surgical site and unexplained drops in the blood hemoglobin and hematocrit levels, the infection went undiagnosed and untreated, and thereafter, became necrotic. Rubins leg was amputated above the knee. Statistically, due to the serious diabetic condition and arteriosclerosis, Rubin may arguably have lost his leg within a five year period. However, with the undiagnosed, untreated infection, the amputation became a certainty. The case settled for $1 million dollars before trial.
Three Minor Boys v. Boy Scouts of America Settlement on Eve of Trial: Amount confidential SEXUAL MOLESTATION Three Cub Scouts living in the South Side projects were sexually molested by their Scout Leader/Sunday School Teacher during scout meetings at the local church. The case settled after long and extraordinarily contentious litigation.
Estate of Michael Hernandez v. City of Chicago Settlement on Eve of Trial: $951,500.00
SIGN MAINTENANCE We alleged that after a road construction project, the City of Chicago forgot to replace "Do Not Enter" signs where a two way street turns into a one way street. In late November of 1990, a young driver continued beyond that point the wrong way on the one way street and collided with another vehicle who was not expecting a car coming the wrong way down the one way street. The first vehicle then struck Michael, a 10 year old boy, who was returning home from school for lunch. The family contacted the Chicago Bar Association who put them in touch with our office. We went out to the scene immediately and found a Do Not Enter sign located on the right hand side of the road which appeared to be freshly installed, given fresh footprints at the base where it appeared the street workers had stomped down the dirt. Also, adding to our suspicions, a handwritten date of 12/90 was written on the back of the sign. (We believe the notation was left by one of the City workers for anyone investigating the case as a matter of a street justice code of honor, although we have no firm evidence as to this point.) Initially, the City denied our allegation that no signs were in place. However, in discovery, we found a pre-construction photograph that showed a Do Not Enter sign located on the left hand side of the road, but not on the right hand side. And, as the case progressed, we uncovered a Polaroid photograph taken on the date of the occurrence demonstrating that there were no signs up at all at the time of the incident.Quentin Turner v. Ingalls Memorial Hospital Settlement on Eve of Trial: $900,000.00
MEDICAL MALPRACTICE The physician failed to properly identify and treat gestational diabetes and macrosomia during the prenatal and perinatal periods of his mother's pregnancy, which resulted in a brachial palsy injury to the child. The physician, in deposition, initially denied there were symptoms or signs consistent with these conditions, asserting his prenatal chart supported his claim. In part two of the physician's deposition, we proved that the obstetrician had changed his prenatal chart to eliminate the evidence. We had discovered that the copy of the prenatal chart forwarded to the hospital weeks beforehand had been altered to emulate the alterations made in the physician's chart. The case settled shortly after the deposition concluded.William Lively v. Certain Confidential Medical Center Settlement on Eve of Trial: $850,000.00 (Randolph County) MEDICAL MALPRACTICE Mr. Lively, a 74-years-old man, was admitted to the hospital February 2, 2005 for a scheduled colostomy reversal. A surgical sponge was negligently left in Mr. Lively's abdomen. The sponge remained in Mr. Lively's abdomen during the course of his nine day admission before the retained sponge was finally identified. The retained sponge caused a myocardial infarction which arose due to sepsis and the trauma of additional surgery; development of deep vein thrombosis (blood clots), gall bladder inflammatory problems with biliary stasis and sludge, urinary tract infection, renal failure, ileus, chronic venous insufficiency, and the lack of reserves to compensate for the insufficiency also arose as a result of this incident.
Estate of Linda Nickerson v. Michael Reese Hospital Settlement: $825,000.00 MEDICAL MALPRACTICE The hospital and its physicians failed to timely identify and treat post-surgical bleeding after laparoscopic surgery for an ectopic pregnancy. Mrs. Nickerson bled out and died.
Diminskis v. Chicago Transit Authority (tried with Howard Schaffner) Jury Verdict: $800,000.00 BUS/PEDESTRIAN COLLISION In February 1983, Mr. Diminskis, a 75 year old, was in route to his part-time job at the Draugus Lithuanian Bookstore and was crossing eastbound across Western Avenue at 73rd Street when he was struck by a C.T.A. bus. The injuries resulting from this accident included a subdural hematoma which required surgical evacuation. The C.T.A. driver insisted that Mr. Diminskis darted in front of the bus. Mr. Diminskis, due to his injury, had no recall of the incident. The fact the driver had been suspended after the incident was barred from the evidence as a post-trial remedial measure.
Estate of Donald Mazique v. Mt. Sinai Hospital Settlement: $700,000.00 MEDICAL MALPRACTICE The physician failed to properly identify and treat fetal distress, which resulted in a stillborn birth.
Brian Harrington v. Ademola Adekola Settlement on Eve of Trial: $500,000.00
MEDICAL MALPRACTICE Brian Harrington, an adolescent, stated that he was riding on the apartment building's freight elevator when it unexpectedly started jumping up and down. Brian tried to get off the elevator when it stopped between floors. When it began to move again, it caught his leg between the wall and the floor of the elevator, tearing his calf muscles. The defense denied that the boy's story was plausible or even possible The case settled within a week of the court ordered experts' inspection, when both the defense and plaintiff's attorneys and their experts were trapped in the same elevator when it stopped and began jumping up and down exactly as described by the plaintiff in his deposition. Fortunately, for the attorneys on the elevator during the inspection, the two experts (one for the plaintiff and one for the defense) were able to disable the elevator to allow everyone to exit it safely, although it did take several minutes to do so.Estate of Kutilek v. City of Chicago Settlement: $500,000.00 total, $315,000.00 to estate
ROAD DEFECT A 23 year old woman and her friend were attending Dick's Last Resort at North Pier. A canal known as the Ogden Slip behind North Pier dates back to the 19th century when the City fathers intended on cutting numerous canals along the north side of the City to take advantage of the City's waterways. After this canal was cut, the age of railroad came, making the canal plan obsolete. The canal was adjacent to the original homestead area of Jean Baptiste Pointe du Sable, the first non-native settler of Chicago, which land was later sold to Chicago Dock and Canal Trust. The land was originally for industrial use and, in the years before the incident, was the City's street salt pile. Unfortunately, the area underneath Lake Shore Drive was open, and Ms. Kutilek after leaving the aforesaid establishment found herself on the service road under the Lake Shore Drive structure. As she operated her vehicle northbound, she drove her vehicle into the canal. We claimed that the lay of the road made it appear that the road continued on to the north, because the roadway north of the slip rises giving the appearance of continuity. The City claimed the incident was the result of alcohol consumption.Sharon Hernandez v. Joseph Thomas, M.D. $449,206.50 (Jury Verdict: $383,000.00 + additional settlements)
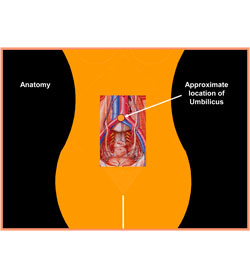
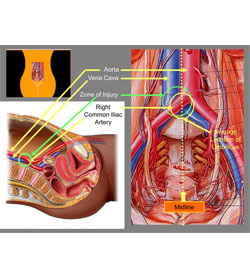
MEDICAL MALPRACTICE The case arises out of a gynecology hysterectomy surgery on March 31, 2010, during which there was a surgical misadventure wherein Mrs. Hernandez sustained severe abdominal bleeding due to iliac artery and vein and small bowel lacerations occurring on the placement of a laparoscopic trocar. Due to severe blood loss, Mrs. Hernandez went into cardiac arrest. A code blue was called and Mrs. Hernandez was given massive blood product augmentation to compensate for the bleed. Subsequently, surgical repairs were performed to the small bowel mesentery and internal iliac artery and vein. Within a day after being discharged home, Mrs. Hernandez was re-hospitalized at Advocate Christ Hospital for blood clots relating back to the misadventure. Mrs. Hernandez was on blood thinners for a year. Additionally, approximately a year after the surgery, Mrs. Hernandez was advised that one of the donors of the blood products she was required to receive due to the surgical misadventure was HIV positive. Although Mrs. Hernandez did not ultimately develop an HIV infection the close brushes with death led to the development of Post-Traumatic Stress Disorder. Before inserting the laparoscope, a primary cannula (or port) must be positioned in the abdominal wall to establish access to the peritoneal cavity. In open laparoscopy, initial entry into the peritoneal cavity is achieved with the creation of a “minilaparotomy” typically using either a transverse subumbilical or midline infraumbilical incision down to the rectus fascia to gain entry into the peritoneal cavity. ,In such instances the cannula is fixed into position with sutures or other suitable techniques. Closed techniques are blind approaches where the cannula is introduced without the minilaparotomy. For this technique the cannula is usually fitted with an obturator designed to penetrate the abdominal layers. This process may be accomplished following the creation of a pneumoperitoneum by the instillation of carbon dioxide gas via an insufflation needle also passed blindly, or it may occur without such inflation; a technique called “direct insertion”. When performing the closed, preinsufflation technique, insertion of the insufflation needle and primary cannula is aided by an understanding of the normal underlying anatomy, especially the location of the larger retroperitoneal vessels. A “safety zone” exists inferior to the sacral promontory in the area bounded cephalad by the bifurcation of the aorta, posteriorly by the sacrum, and laterally by the iliac vessels. In women placed in the Trendelenberg position, the great vessels are oriented more cephalad and anterior, making them more vulnerable to injury, a circumstance that may or may not be mitigated by adjustments in the angle of insertion. Therefore, positioning of the insufflation needle and the primary cannula are best accomplished with the patient in an unaltered supine (horizontal) position, and the surgeon should avoid insertion in the Trendelenberg position. We argued that Dr. Thomas failed to possess and use the knowledge, skill, and care ordinarily used by a reasonably careful physician practicing Obstetrics and Gynecology by performing the technique for primary closed or blind access to the peritoneal cavity after placing Mrs. Hernandez in the Trendelenberg position, contributing to cause her injuries. The defense denied that there was a deviation from the standard of care and argued that the bleeding incident was a known risk of the surgery. The insurance company for the physician offered zero dollars to settle the case. The jury disagreed with the insurance company evaluation and returned a substantial verdict for the familyEstate of Doris Hoppe v. Edward Hirsch, M,D., et al. Jury Verdict: $ 389,700.00 (Dekalb County) MEDICAL MALPRACTICE The physician failed to diagnose and treat a bleeding ulcer in a 68 year old woman, resulting in her death. The insurance company for the physician offered zero dollars to settle the case, perhaps because the case was being tried in rural DeKalb County, Illinois where no one had previously won a medical malpractice verdict or obtained a six figure verdict. The jury found in favor of the Hoppe family members despite the fact that several of the jury members were patients of same medical group or socialized with the defendant doctor.
Yoon v. Jones Truck Line Jury Verdict: $383,915.00 for occupants of the automobile AUTOMOBILE/TRUCK COLLISION In January 1982, Miss Yoon and her boyfriend were driving at 3:00 a.m. during a sleet storm on I-55 twenty miles south of Joliet. The roadway was passable only in two tire ruts in the right hand lane. As her boyfriend attempted to pass a truck using the left hand lane covered with sleet, he lost control of the car and struck the left guard rail of the Mason River Bridge and spun back into the road. The truck driver claimed that the car passed him at 70 m.p.h. and that just before the collision, the car backed up, swerving to face the truck and blinded the truck driver with its bright lights on, just before accelerating the car into the truck drivers path. Although it was clear from the skid marks in the sleet shown in the Illinois State Police photographs that the automobile had lost control in the ice while passing, it was also apparent from those same photographs that the truck driver was less than candid when he claimed that he was blinded by the bright lights of the automobile. The headlights of the car were seen in the photographs at the initial impact with the guardrail, and therefore, were not on the car at the time of the collision to blind the truck driver or otherwise light up the road. The verdict in the Yoon case included a $151,455.00 award for the Yoon family and was one of the first verdicts in Illinois using as its primary basis for recovery the new component for wrongful death of loss of society following, what was at that time, the new precedent of Prendergast v. Cox, 470 N.E.2d 34. Prior to this, a recovery for the wrongful death of a child required a showing of economic loss in terms of loss of future contribution to the parents, an illogical damage premise.
Estate of Arvid Malmquist v. Village of Lincolnwood Jury Verdict: $238,990.00 BUSH OBSTRUCTION The decedent's wife broadsided another vehicle at an uncontrolled intersection, and the collision caused her husband's head to hit the dashboard. Under Illinois law at that time, if the beneficiary (the wife) was contributorily negligent, that negligence acted as a total bar to recovery in a wrongful death case. The Village's insurance company offered zero dollars to settle, but the jury found that the Village's failure to maintain bushes at the intersection precluded her from observing the other vehicle passing through the intersection, and they returned a verdict on her behalf. The verdict (preceded by Yoon case that was tried in 1986) was one of the first verdicts in Illinois where the majority component for wrongful death was loss of society following the new precedent of Prendergast v. Cox, 470 N.E.2d 34.